How I Diagnosed and Treated My Case of B. Pertussis, aka "Whooping Cough"
DIAGNOSIS
Obvious, But Difficult to Get Confirmed
The cough is the most obvious symptom. It is an uncontrollable choking cough that can make it hard to breathe. At the end of the cough when you try to inhale your windpipe may be blocked by the Larynx closing up (a laryngospasm), resulting in a “whooping” sound, although that is not always present. If you have a violent, intermittent cough like this, odds are you have Pertussis. If you want to convince the doctors try to capture it on video. I kept my cell phone with me and also setup a video camera with infrared at night to capture night-time episodes.
Doctors may be dismissive
Despite the obvious cough you may find your doctors are dismissive because they haven’t seen you cough, haven’t seen a Pertussis patient before, or still incorrectly think of Pertussis as a childhood illness that has been largely eradicated by vaccine. You may have to be very persistent and twist some arms in order to get the tests needed to confirm the diagnosis.
Tests You Should Get
The first test is best to get early on, and the second one is better later in the disease. I recommend asking for both, but if you can only get one get the blood test because it is more reliable.
Test 1: Nasopharyngeal swab with PCR
The nasopharyngeal swab with PCR is useful early in the disease if you have not yet taken antibiotics, but it is hard to do properly and often comes back falsely negative. Basically, they stick a swab all the way up your nose to capture the bacteria, culture it for several days, and clone the DNA by PCR. If done properly and early enough it can confirm the presence of Pertussis. But in many cases (including mine) it is done too late, the swab is not held up the nose long enough, or the culture medium is incorrect, and it returns a false negative.
Test 2: Blood antibody test
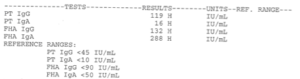
My blood showed Pertussis anti-bodies confirming my diagnosis.
My blood showed Pertussis anti-bodies confirming my diagnosis.[/caption]
The blood antibody test is effective a couple of weeks into the disease and beyond, once your body has begun to mount a defense and around the time you’ve started the nasty coughing. It’s a simple blood draw that is sent to a lab where they will check for antibodies to the Pertussis toxins. This test is much more reliable than the swab and it confirms that you were either just recently inoculated with the vaccine, or else infected with the disease. My case was confirmed with the blood test results at right.
Chinese Medicine
Ancient Chinese medicine is recognized for multiple contributions to modern medicine. These include the discovery of circadian rhythms, benefits of nutrition, recognition of diabetes, isolation of sex hormones, and use of herbs such as Salicylic acid (precursor to aspirin) to treat disease. I never thought to consult Chinese medicine about Pertussis, but fortunately Google did!
Yellow Tongue

Pertussis turned my tongue yellow.
As my cough subsided, I noticed a strange new symptom: my tongue turned yellow. The medical websites were not too helpful but Chinese Medicine notes that a yellow tongue is a symptom of Pertussis. Also of interest, a paper published in Nature’s Scientific Reports determined via molecular scientific techniques that a yellow tongue was associated with the Bacillus genus of bacteria. This is a different genus than Pertussis but it lends credence to the tongue color as a diagnostic criteria for bacterial infection.
Stuff to Skip
Once you are in the hospital lots of doctors will show up to treat you. Some of them turned out to be of questionable value to me. In no particular order:
- ENT scope — This involved putting a scope up my nose and down my throat so the ENT could get a good look at what was going on. It’s not an unreasonable idea, but I suspected it would show nothing, and it did. Despite the lack of evidence the ENT still incorrectly diagnosed Laryngophasal reflux (LPR). Since that would be her diagnosis even without evidence it seemed like an unnecessary procedure, and it caused the other doctors to fixate on the wrong thing. One thing I will say is that she was very good with the scope, and it didn’t hurt. So if you do decide to do one, you probably want it done by the ENT doctor.
- GI scope — This involved putting a scope down my esophagus to look for reflux in the upper digestive tract. This is a much more expensive and risky procedure as you are going under anesthesia. I was particularly concerned about a Laryngospasm while under, and notified the anesthesiologist to prepare for one. Indeed, it happened, and he was ready with an extra dose of proponyl glycol. Although the procedure went smoothly it was an unnecessary intrusion that produced no evidence of gastritis yet still resulted in the GI doctor claiming GERD to be the culprit. If you really think GERD is the issue you can just try the Proton Pump Inhibitor medication that treats it and see if it helps. No need to put yourself at risk just to appease the GI doctor.
- Pulmonologist — I saw two of them (not by choice) and they were completely worthless. One of them did not want to review videos of my cough and instead wanted to discuss possible causes of anxiety, while the other wanted to argue that it couldn’t be Pertussis and I was not the right person to figure out my illness because I had the mind of an engineer not a doctor. Neither of them did any more than listen to my lungs, which were always clear. I’m sure they were paid well, however.
- Speech Pathologist — This lady was very nice and suggested some things to manage the coughing episodes, but they were all things I’d found out on the internet already. Basically, try to breathe through your nose, or control your breath out through your lips. It was nice of her to stop by but I don’t think this made much difference.
The Misdiagnosis You May Get: GERD
Despite all my obvious symptoms, contrary evidence, and the opinion of an expert on Pertussis, the only diagnosis I could get was GERD: Gastroesophageal reflux disease. And also LPR, laryngopharyngeal reflux. Why are doctors so obsessed with GERD? And what connection could there be with Pertussis?
If all you have is a hammer
I can’t say why the doctors fixated on GERD in the face of contrary evidence, but I have a few guesses. The first is how the medical system works. Basically, it’s divided into specialists. Each doctor is an expert in a tiny part of your body, and focuses exclusively on that. When you have a complaint about your throat, coughing, and swallowing, an ENT will get involved. And what an ENT is equipped to diagnose is limited to a few things, including GERD. So she will get out her scope, perform her procedure, and diagnose GERD. That is what she does.
It seems more likely
There is a common medical school mantra that goes like this: “If you hear hoofbeats, think horses, not zebras.” The idea is to go with the more common cause, not the exotic one. And no doubt there are far more cases of GERD than Pertussis going around. However, there should probably be a corrallary that goes like this: “If the horses have stripes, they may actually be zebras, not striped horses.”
A Possible Connection with Pertussis?
For many years, ulcers were thought to be caused by “stress”. Then doctors discovered the H. pylori bacteria. Surprise, it was not just “stress” putting holes in people’s stomachs! GERD strikes me as something similar. It is often said to be caused by stress, or spicy foods, but I wonder if a bacteria might also be involved. Plenty of websites implicate H. pylori in GERD. But I also noticed a connection between Pertussis and Bacillus. Although one is a gram-negative bacteria and the other gram-positive, it is interesting that they both produce a yellow tongue and are treated with the same herbal decoction in Chinese medicine. Further, the Bacillus infection underlies the Chinese version of GERD, called “Chronic Erosive Gastritis” or CEG. Is it too much of a stretch to think that the Pertussis bacteria might also irritate the digestive track with its various toxins and produce GERD-like symptoms?
Disclaimer – I am not a doctor and this is not medical advice! But you may benefit from my experience.